Guillain-Barre Syndrome: What You Need to Know
Guillain-Barre Syndrome (GBS) can feel like a sudden, scary roller‑coaster. One day you’re fine, the next you notice tingling in your feet or weakness that spreads upward. It’s not a disease you catch like a cold; it’s an autoimmune reaction where your body mistakenly attacks the nerves that control movement and sensation. Most people hear about GBS after a recent infection—like a stomach bug or flu—so the timing can be confusing. Understanding the basics helps you spot red flags early and get the right care fast.
What Triggers Guillain-Barre Syndrome?
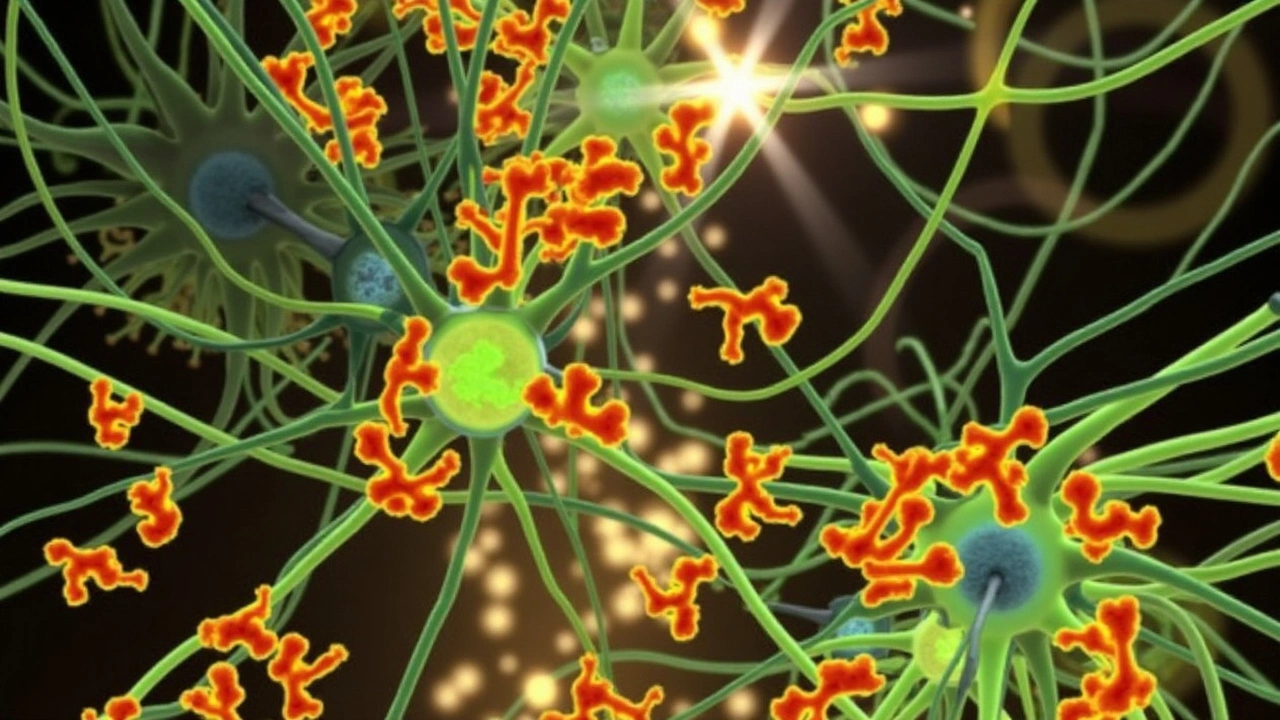
Although doctors still piece together the exact cause, about two‑thirds of GBS cases follow an infection. Campylobacter jejuni, a bacteria that causes food‑borne illness, tops the list. Respiratory viruses, such as the flu or COVID‑19, are also common culprits. In rare cases, vaccinations or surgery can set off the immune response. The key point is that the trigger isn’t the problem itself; it’s the body’s over‑reaction that damages the myelin sheath around peripheral nerves. This damage slows or blocks the signals that tell muscles to move, which is why weakness spreads quickly.
Spotting Symptoms Early
GBS usually starts with a tingling sensation in the toes or fingers. Within days, that numbness can turn into muscle weakness that climbs up the legs, arms, and sometimes the face. If you notice trouble climbing stairs, gripping objects, or walking without stumbling, it’s time to see a doctor. Some people also experience pain, difficulty breathing, or problems with bladder control. The progression can be rapid—sometimes hitting its peak within two weeks—so don’t wait for the symptoms to worsen before seeking help.
Doctors diagnose GBS through a combination of a physical exam, nerve‑conduction studies, and a spinal‑fluid tap (lumbar puncture). The fluid often shows elevated protein levels with normal cell counts, a classic sign of GBS. Early diagnosis is crucial because treatment works best before the nerves suffer long‑term damage.
Treatment Options and Recovery Tips
There are two main treatments: plasma exchange (plasmapheresis) and intravenous immunoglobulin (IVIG). Both aim to reduce the harmful antibodies that are attacking the nerves. Treatment usually lasts a few weeks, and many patients start to improve within a month. Physical therapy is a big part of the recovery plan—gentle exercises keep muscles from atrophying and help restore coordination.
Recovery timelines vary widely. Some people bounce back completely in three to six months, while others may need a year or more for full strength. Staying hydrated, eating a balanced diet, and getting enough rest are basic but powerful ways to support the healing process. If breathing becomes difficult, hospitals can provide ventilatory support, which can be lifesaving.
Living with GBS also means watching for potential setbacks, known as relapses. Though rare, they can happen, especially if the immune system gets another trigger. Keeping follow‑up appointments with a neurologist and reporting any new symptoms early can prevent complications.
In short, Guillain-Barre Syndrome is a serious but treatable condition. Spotting the early signs, getting prompt medical care, and staying active during recovery can make a big difference. If you or a loved one experience sudden weakness or tingling, don’t ignore it—call a healthcare professional right away.
Maharashtra Faces Urgent Health Challenge as Guillain-Barre Syndrome Cases Rise to 101 in Pune
Maharashtra is grappling with its first reported death due to Guillain-Barre Syndrome (GBS) amidst a surge of cases reaching 101 in Pune. The deceased, a resident of Solapur, showed symptoms typical of GBS before passing away. This alarming situation has prompted authorities to undertake extensive water testing and launch public health surveys. The state's response includes the deployment of a seven-member expert team to curb the spread and provide necessary medical support.
VIEW MORE